If we had to open the heart of a nurse, we would see many things like compassion, empathy, and love. Now more than ever, these loving people are often placed in situations that can compromise their safety.
Growing up in some of the toughest streets in Hialeah, FL in the late 60s early 70s and as a veteran of the United States Marine Corps, violence was a part of my everyday life. By the time I was in 3rd grade, I was desensitized to a lot of violence.
Today, I want to focus on improving the safety of these compassionate, empathetic and loving people we call nurses. I would like to share why nurses are so important to me. As I mentioned before, I grew up in some of the toughest streets in Hialeah, FL. My mom died at a very young age from drug use. And when you put drugs in your body, you often end up in the emergency room one way or another. Between third grade and sixth grade, I spent more time in the emergency room waiting for my mom to be discharged or committed to mental health or a rehab center, than I spent in school. Often, I would sit in the emergency room with my younger brother, who was in the first grade at the time, just waiting for child services to show up, not knowing what else to do.
I’ll never forget Nurse Samantha Jones. I was often met with a smile and a friendly hug from Nurse Jones. Many times, she would offer me a cup of juice, a candy bar, or even a sandwich. I was amazed at how she would greet me and then moments later return with something to eat. She just knew I needed something, especially when she would see me break off half of whatever she gave me to share with my brother, and she watched how quickly we devoured it.
Eating wasn’t something we did on a regular basis. Nurse Jones had such a way of quickly turning my frowns upside down. Our friendship grew to watching me play sports and graduating high school. Years after my high school graduation, I found out she had passed away. So, in my heart, all nurses rock!
Realities of Environmental Risk
According to the American Nurses Association, 1 out of 4 nurses are assaulted on the job. Further, 76% of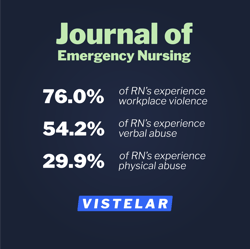 registered nurses report experiencing workplace violence according to a 2014 study published in the Journal of Emergency Nursing. The study found that 54.2% of nurses experienced verbal abuse from patients and 29.9% experienced physical abuse. Today, there is the additional frustration and anxiety caused by the COVID-19 pandemic. As we are seeing around the country, these ingredients can quickly escalate into acts of violence with little to no warning.
registered nurses report experiencing workplace violence according to a 2014 study published in the Journal of Emergency Nursing. The study found that 54.2% of nurses experienced verbal abuse from patients and 29.9% experienced physical abuse. Today, there is the additional frustration and anxiety caused by the COVID-19 pandemic. As we are seeing around the country, these ingredients can quickly escalate into acts of violence with little to no warning.
It is possible to manage your safety and still be compassionate. The first thing you will do begins at 10 feet away, or when you initially make eye contact with the person you are going to be engaging. For example, at 10 feet when you are standing at the doorway of the patient’s room, you quickly conduct a risk assessment of the immediate area beginning with the walls, floor and contents in the room. You look around the room to make sure that curtains are open if they’re supposed to be, blinds are drawn if they’re supposed to be, windows are closed and locked as they should be. Check the walls for damage, spilled beverages, or thrown food that might have happened before you arrived. Take notice if the bathroom door is open or closed. Ensure that everything that is supposed to be plugged in, is plugged in. Is the trash can where it’s supposed to be? Is there any debris, clothing, shoes, food, utensils or pens on the floor as we make our decision to approach? Is there a chair in the room? Does it have anything on it such as a jacket or a sweater or a purse or bag? This could be an indicator that there may be an unexpected guest in the room.
Then we shift our attention to the patient. Are they secured properly on their bed under the covers? Can you see their hands and arms from the doorway? Is there an I.V. or any testing cables from the wall and are they properly connected? Check the patient’s facial expressions if possible. Are they happy to see you or are they unhappy to see you? Are they showing concern? The biggest question to ask is, does their emotional state of mind match the situation that they are in? All of these can be indicators to help you assess for safety prior to making contact.
If for some reason you do not feel it is safe to approach, then it would be in your best interest to stop and call for additional assistance.
Universal Greeting
Once you feel it is safe from that distance, the next position is just as important; walk to the foot of the bed and stop. This will give you the best possible position to manage your safety and apply your verbalization skills with the Universal Greeting.
 The universal greeting is one of the most powerful tools a health care professional has when engaging with the patient, family members or even other staff. It allows you to establish a social contract of fairness and respect while showing them that we are all equal in this together. After we give them our universal greeting, we want to gauge their level of response to us. Are they lying there calmly responding to us, or are they extremely fidgety? Look closely at their hands and make sure you can see them. Are they tucked under the covers? Can or did they kick their legs free from the covers?
The universal greeting is one of the most powerful tools a health care professional has when engaging with the patient, family members or even other staff. It allows you to establish a social contract of fairness and respect while showing them that we are all equal in this together. After we give them our universal greeting, we want to gauge their level of response to us. Are they lying there calmly responding to us, or are they extremely fidgety? Look closely at their hands and make sure you can see them. Are they tucked under the covers? Can or did they kick their legs free from the covers?
Are they looking directly at you with inappropriate facial expressions or engaging you cooperatively? Do they appear to be disoriented, confused and haven’t even identified you being in the room yet? If you feel this position at the foot of the bed is not safe to continue, you will simply exit the room to get additional help to assist you with your contact.
If you do feel it is safe to move closer, then you would go to the appropriate side of the bed.
There’s a reason why conducting a risk assessment, in this fashion beforehand, is very valuable and important no matter how much time you feel you have or don’t have. My daughter is a nurse; on her first day, I received a call from her telling me that she walked into a room to take a patient’s vitals and check on their wellbeing, and the patient bit her! I asked her what she did before being bitten.
She said, “I just walked in the room like all the other nurses. I said, ‘hello’ and when I went to adjust the covers, he reached up and bit me in the arm”. When I had her think about what had happened and asked her to consider the tactics I shared above, did she believe that the bite could have been avoided? Yes, she did. So, my question to you is, what routines are you using to help manage your safety or has your safety routine just been made of luck? Will the above strategy help you stay safer?
Developing an Exit Strategy
Next, you must develop an exit strategy for when you need to quickly terminate a contact for emergent reasons, such as your personal safety. These exit strategies are a list of reasons you will prepare ahead of time so you can explain why you need to leave an area immediately. For example, if you are engaged with a patient, and you feel it is unsafe due to their mannerisms, aggressive words, or actions, simply place your hand with your palm facing them, and say, “I know this is important to you, but I have to go assist another nurse right now. I’ll be right back”. Then leave the room. Another exit strategy could be if you’re filling out information and you realize the patient is being very uncooperative, which might compromise your physical safety, just tell them your pen ran out of ink and you’ll be right back. This will allow you to leave the area and keep your professional face, and they can feel respected.
Exit strategies help us to remain professional and allow the patient to keep their self-respect in the process. One of the biggest reasons this is important is because you’re going to see these people again and again and you want to make sure you manage your safety without them feeling disrespected. Exit strategies not only work with patients, but they also work with family members when they are demonstrating at-risk behaviors that may compromise your safety. If you are talking to a family member, and things do not feel right and you need to leave, you could step back and cough into your elbow, tell them that you’ll be right back because you’re not feeling well. Another exit strategy at work could be while you’re engaging in conversation with them, you quickly look behind them and tell them I know this is important to you and I will be right back so we can finish, but I need to speak with this other nurse.
Be Aware of Your Surroundings
The last thing I would like to address is how to avoid getting surrounded. You see, in my life, I have had many physical confrontations that started with one person and ended with five or more. The first thing to do to manage your safety and avoid getting surrounded is to be aware of your surroundings and to keep the person or persons you are speaking to in front of you. For example, if you have two people talking to you and one seems to be trying to get behind you, reposition to essentially put one person between you and the second person there. If the attempts continue, leave the area if possible. Inside of a small room, consider keeping your back towards the open door and exit the room if you feel you’re being surrounded.
We also have a strategy called guiding hands to assist a person to walk with you, while not allowing them to get behind you.
The best strategies in any nurse’s toolbox are to manage their facial expressions, manage their distance from the person or people they are talking to, manage their tone of voice when speaking, remain cognitive of their word choice, and stay aware of their surroundings.
And please remember. All NURSES ROCK!