Enjoy this excerpt from one of our published books.
Chapter 2
Everything is Okay Now. Respond, Don't React
“Violence can only be concealed by a lie,and the lie can only be maintained by violence.”
-Aleksandr Solzhenitsyn
The security team arrived on the unit in just a few minutes, but the floor was already quiet. The call from dispatch said a nurse was being actively assaulted, so everyone double-timed it up to the floor. When they arrived at the patient’s room, the door was closed and they were silently greeted by a doctor and some nurses standing outside. Andrea, the first arriving officer, was also the first to break the silence. “Is everyone okay? What happened?” she asked.
“Everything is okay now,” replied the doctor.
“Well that’s a relief,” replied Andrea. “Is anyone hurt?”
To that, the doctor looked sufficiently annoyed and replied, “Nope. It was just a little misunderstanding. Everything is fine now, so you can all go back to work.”
“Can I at least see the nurse who said she was assaulted? I have a report to write,” replied Andrea, as she stepped toward the patient’s room.
“Is that really necessary?” he said and stepped in front of her.
Concealed inside the room was the startled patient, curled up in her bed, as her nurse lay unconscious on the floor. The visitor who had struck the nurse had fled down a stairwell, just seconds before the security team had arrived. Oblivious to the medical emergency behind him, the doctor continued to argue with the security team, while precious minutes flew by, saying “If you go in there you will only make things worse.”
In his defense, the doctor had no idea the extent of the injuries to the nurse, having arrived just a few seconds prior to the security team. He hadn’t witnessed the assault but was told by the nurses on the unit that there was a fight in his patient’s room. At that moment, he was only operating on a flawed but very common instinct among providers. That instinct was to advocate for his patient, no matter what the circumstances. In his eyes, keeping security and the hospital’s administration out of the provider-patient relationship was his first priority.
The First Responder Philosophy
If he had been trained in the First Responder Philosophy (FRP), his first instincts after he’d arrived would have been to assess the scene by listening, by looking and by quickly asking questions of the nursing staff. Then he would have raised the alarm by calling for security himself. Luckily, someone who was thinking more clearly had already done that. His next step would have been to evaluate the scene to determine if it was safe for him to enter the room alone or wait for the security team.
Then he and/or the security team would enter the room where they would have seen the nurse unconscious on the floor. Their next step would have been to stabilize the scene. Although the perpetrator had already fled, an injured nurse and a frightened patient both needed care. So the physician could have started the next step— an initial medical assessment of the unconscious nurse while other nurses saw to the patient’s needs.
The First Responder Philosophy then would have also triggered the long-term monitoring phase, where the physician would have called for a medical response team to transport the nurse to the emergency department for further treatment. The next step would involve communication between the security team, the police, and hospital administration so the suspect could be apprehended, searched and identified. Finally, the FRP would require that all parties document and debrief the incident, so a risk assessment could be completed, and a safety plan implemented to protect everyone from future risk.
the police, and hospital administration so the suspect could be apprehended, searched and identified. Finally, the FRP would require that all parties document and debrief the incident, so a risk assessment could be completed, and a safety plan implemented to protect everyone from future risk.
The First Responder Philosophy has a long history of improving institutional responses in everything from hospitals to prisons. It safely and effectively guides teams to manage incidents involving fire, medical emergencies, violent disturbances, and miscellaneous incidents, like chemical spills and utility shutdowns.
Since I was first trained to use the FRP in a hospital setting over two decades ago, I have relied on it. It was developed by Gary Klugiewicz, Bob Willis and their colleagues for the State of Wisconsin Department of Corrections. If the physician of our story had been trained in the First Responder Philosophy, things probably would have gone very differently when he’d first arrived on the scene.
Aside from a lack of training in a response model like the First Responder Philosophy, what else might have caused the disconnection between the medical staff, the security staff, and, ultimately, the hospital administration in this instance? Perhaps it was the overall acceptance of violence in healthcare. Certainly, the doctor wouldn’t have barred access to the patient’s room, if the smell of smoke was wafting from the room. Yet, both nurses and patients are injured by violence with far more regularity than fire. Perhaps healthcare professionals must begin to understand that violence is an institutional emergency, just like a fire, flood, or a power outage.
If you still don’t agree that the acceptance of violence in healthcare is one of the cultural drivers that lead us along a path of endemic violence, consider the many general myths people commonly embrace about violence (e.g., “bullying toughens kids up;“ “always smile when dealing with the public”). In this book we’ll discuss seven violence-enabling myths that are prevalent in healthcare.
Myth #1: “If you say something, it will make things worse.”
This one tops the list for me. It’s the myth I hear most often and perhaps the one that does the most damage. If you’ve worked in healthcare for even a short while, you’ve probably heard this one. Worse yet, you’ve probably come to embrace it on some level. So, if you’ve heard this myth, forget it. And, if you hear someone say it, correct them.
The fact is, if we ask someone confidently and respectfully to stop behaving badly, they usually will comply. When we say nothing, while people behave badly in our presence, the non-verbal messages of silence are permission and submission. Specifically, if we say nothing when people threaten or even demean us, the non-verbal messages are, “it’s okay to behave that way” or “I have no authority to act.” Perhaps, the worst of all nonverbal messages is, “I’m afraid.” Failing to speak up when people need limits set on bad behavior usually ensures that we’ll get more bad behavior and that it will escalate.
If the people involved in the angry biker situation had believed this myth, no one would have addressed his behavior, and certainly not with any consistency. What also can be learned from the angry biker is that, if we focus on behavior, the attitude will follow. That is another important principle for establishing a therapeutic relationship. Skilled communicators focus on a person’s behavior, not their attitude. What we do naturally is to focus on a person’s attitude hoping that their behavior will improve. This rarely works and even backfires as the aggressor feels empowered by your attempts to assuage their anger, by incessant apologies, by allowing them to vent, and by otherwise rewarding their bad behaviors. To make things worse, if all you’ve been trained to do is service recovery and/or crisis intervention, then appeasement is probably the only skill you’ve ever been taught.
Myth #2: “Don’t sweat the small stuff.”
Another reason there is so much violence in healthcare is because our definition of violence is too narrow. As already stated, everyone knows not to drop f-bombs in church or talk loudly in a library. But why do so many people yell, curse and threaten in a hospital? Is it simply because some people behave badly when they’re sick? Or is it because they believe they are entitled to behave badly, simply because they’re sick? Perhaps it’s because healthcare workers believe patients have a right to behave badly. In reality, it’s all the above.
Myth #3: “Kill them with kindness.”
This is the myth that goes like this, “Just be nice when people abuse you, because if you’re real nice to them, they will start to like you and stop abusing you.” I call this the myth of submission. Submission is a survival skill. It’s a natural tactic for finding a place in the pecking order of nature. When we behave this way we are telling the person who is behaving badly that they are in charge and that we’re afraid. We can’t answer bad behavior with more bad behavior, so it’s not about challenging the aggressor. It’s about setting the appropriate Social Contract and maintaining it.
Without going into too much detail about this myth, its efficacy can be tested with a question: Would you tell someone involved in a domestic violence relationship to kill their tormentor with kindness? If your sister or daughter told you that their husband or boyfriend was abusing them, would you tell her to just fix herself up and be more romantic? Would you tell her to shower her man with love and attention? Of course you wouldn’t. Then why do we keep giving each other essentially the same bad advice in healthcare?
Myth #4: “People behave badly because they are sick and under stress.”
Is this really true? Cumulatively, I’ve spent hundreds of days of my life in acute care as a consumer. I once spent a month in a hospital recovering from a painful and complex orthopedic surgery. My son has had five operations in total. My father had several cancers, before liver cancer finally took him. My late wife had a twenty-year long chronic and severe health condition, before it finally took her. In all that time, through all that stress, fear and pain, I never yelled at, cursed at, or threatened a healthcare provider.
Does that make me special? Absolutely not! In fact, the majority of people who visit our clinics and hospitals everyday never threaten us or otherwise behave inappropriately. It’s only a small number of people who make the healthcare environment uncomfortable and unsafe. Sure, perhaps people are more likely to act out when under stress. No one wants to be in a hospital. Everyone there is either sick or connected to someone who is. That said, if we set limits on behaviors effectively and provide the kind of support that people in crisis really need, then we can have more peaceful and therapeutic environments of care for everyone.
Myth #5: “Violence is just part of the job.”
We’ve got to stop saying this, because this myth is literally killing us. I’ve heard this one since the first day I started working in healthcare in 1991. Just like in any other cycle of violence, if we accept this myth, we are paralyzed to act and doomed to remain victims. Because so many people embrace this myth, the majority of schools are unsafe for many children who find themselves endlessly bullied and hopeless. Because of this myth, residents and staff of group homes for people with psychiatric conditions and brain-based disorders are commonly locked in a daily cycle of violence and fear. And staff are assaulted on the job at rates at least seven times more than average.
Why is it that if a nurse threatened a patient we would fire him or her without question? But when a patient threatens, shoves, spits at, and perhaps even slaps a provider, we are hesitant to even call security? It’s partly because of this pervasive and destructive myth. Abraham Lincoln once said, “Familiarize yourselves with the chains of bondage and you prepare your own limbs to wear them.” His point was that if all are not free then none of us are assured of our freedom. Likewise, just as we must ensure the safety of our patients we must ensure the safety of our providers. But we’ll never get to a safer place in healthcare until we can at least agree that a safer place exists!
If we can’t eliminate disrespect and fear for healthcare providers, then we cannot eliminate them for our patients either. Peggy Troy, the CEO of Children’s Hospital of Wisconsin, is fond of saying “The patient experience cannot surpass the employee experience.”
She understands the experience of the patient and the provider are inextricably bound together. Unfettered anti-social behavior not only leads to violence, but it sours the environment of care for everyone—staff and patients alike.
Myth #6: “The Customer is Always Right”
Almost one in three surveyed emergency department and family practice physicians has admitted to prescribing antibiotics to patients who didn’t need them, even though everyone knows the overuse of antibiotics is a threat to public health! Even more shocking, two out of three surveyed doctors have admitted to delaying vaccines in pediatric patients due to unscientific and misguided beliefs embraced by their parents. Sadly, most of them did so knowing full well that it was unhealthy for their patients and for public health. As a result, the CDC fears that measles and whooping cough are back with a vengeance and probably more resurgences of dangerous diseases in children are yet to come. Why? The reason most often given by physicians was pressure from their patient’s parents.
Somewhere along the line, we started treating healthcare like retail and not as a profession of higher calling. Yes it’s a competitive environment, but where do we draw the line? I propose the line exists where unscientific notions impinge on the interests of patient care and public health. Perhaps we can start by ceasing to view patients as merely customers. The “customer” isn’t right when they impinge on the rights of others. And, if the “customer” is endangering their own health or that of others by acting against medical advice, providers have to persuade and educate them. But that takes training and a new way of doing business.
The best place to start is to rediscover our professionalism in healthcare. A hospital is not a department store. It is an institution of healing and education. If so many doctors are failing to influence the healthcare decisions of their patients, then perhaps communications training, and not crisis intervention theory, is the answer.
Myth #7: “Things really aren’t that bad.”
Once while I was waiting to meet with a physician and his staff about a patient who had threatened his life, I struck up a conversation with one of his nurses. I asked her if anything like this had ever happened before. She said it hadn’t and that she was in shock over the whole incident. Nonetheless, she thought the whole thing was silly and that the doctor was making way too much of things.
I then asked her how long she’d been in nursing. She explained she’d been a nurse for more than 30 years and worked in many specialties, as an RN and Master Degree prepared nurse. I then asked her if she’d experienced much violence on the job. She replied, “Not really. Things really aren’t that bad. A little conflict here and there is just part of the job.” I then asked her if a patient or visitor had ever shoved her, and she said “sure.” I then asked her if anyone had ever slapped her and she said, “I’ve been slapped a couple times, sure.” I asked her if she’d ever been kicked, punched, grabbed, or spit on and she answered yes to all. Finally, I asked her what sort of behavior did she consider to be violent. She replied, “Yeah, I see where you’re going, but I used to be an E.R. nurse. A lot of that stuff happened there. After that, I would only get attacked by someone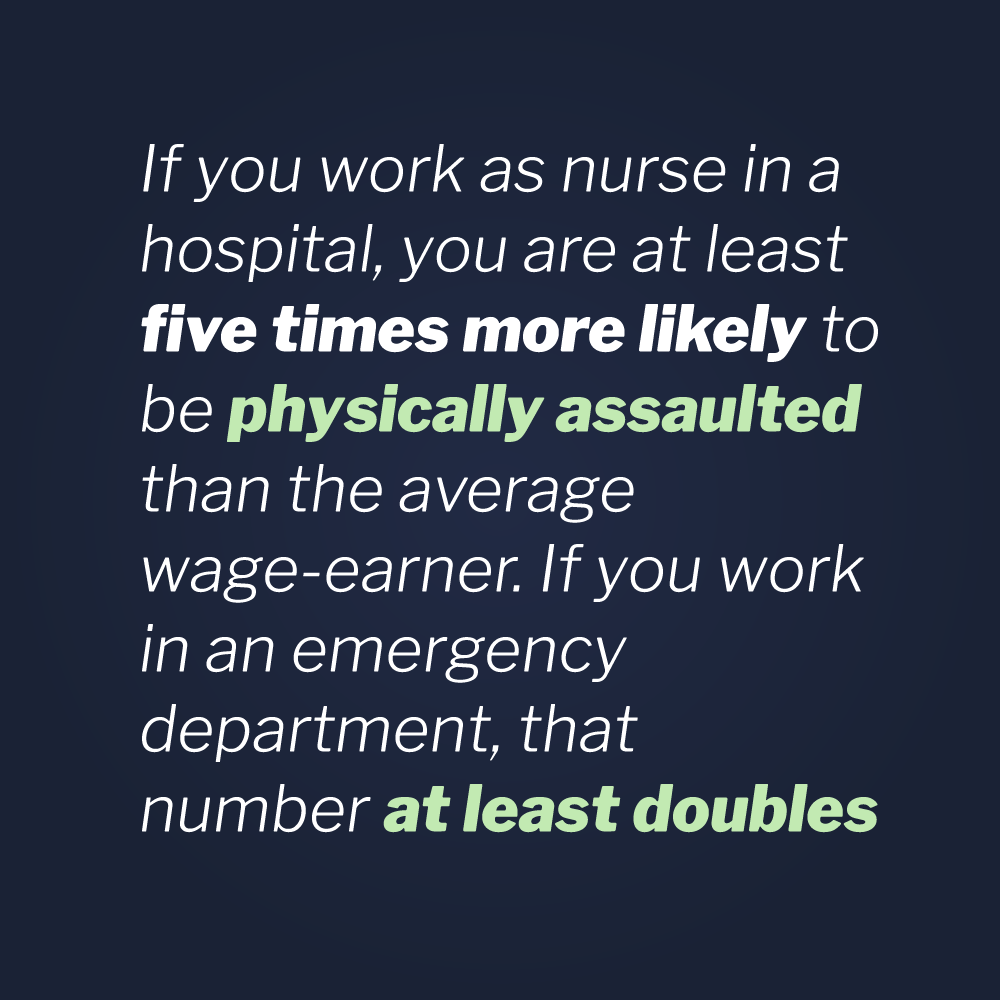 once in a blue moon.”
once in a blue moon.”
As previously stated, if you work as nurse in a hospital, you are at least five times more likely to be physically assaulted than the average wage-earner and if you work in an emergency department, that number at least doubles. We need to act now. It’s time to ask ourselves if this is really the way it has to be. Are we getting anywhere by denying there’s a problem? Are we getting any safer? Have our notions of family-centered care and the old methods of crisis prevention even made a dent or are they propagating and perpetuating the very same mythology that keeps us locked in a cycle of violence? So what is the solution? Perhaps one can be found among the seven answers to the seven myths of violence in healthcare.
All of the skill sets described in this book are intended to develop a pre-planned, practiced, response in the practitioner, so that they can successfully manage conflict and treat their patients. In order for them to be successful, the institutions they work in must support them by creating an environment of care that is incompatible with anti-social and violent behavior. In answer to the seven myths, the following seven steps prepare a hospital or clinic to begin constructing a safer and more therapeutic environment.
Step #1: Create the expectation that everyone must Take Appropriate Action whenever anti-social and violent behavior is observed.
Healthcare workers have to adopt a “hear something — do something” mentality when it comes to violence. They must be trained to consistently address the Gateway Behaviors of Violence when they see and hear them, then Take Appropriate Action. They also must learn to judge whether to take action with their co-workers and when it’s necessary to call security or law enforcement. The concept of when word-based tactics fail will be discussed in a later chapter.
Step #2: Adopt a clear and broad definition of violence.
Because violent behavior is connected through gateway behaviors, we need to include anti-social and threatening behaviors in our definition of violence. Also the refusal to follow basic policies and procedures by patients and visitors should not go unnoticed and unanswered, even if we don’t directly identify such resistance as violent behavior. If we can’t get someone to comply with something as seemingly insignificant as wearing a visitor’ pass, then how do we expect to persuade them to cooperate when the stakes are even higher?
At the very least, a clear definition of inappropriate and violent behavior in a hospital should always include behaviors that disturb or offend others, such as: demeaning language or comments regarding a person’s race, religion, sexual orientation, age, body shape; profanity, swearing or cursing; shouting, yelling, or loud talking; implied or overt verbal threats; sexual comments and unwanted advances; touching without permission (unless necessary for the safety of self or others); behavior that disturbs others or causes fear, in patients, visitors, and staff.
Step #3: Train providers and staff to perform non- escalation skills.
Non-escalation is a unique skill set that practitioners of Vistelar’s conflict management methodologies practice and learn in scenario- based drills. Gary Klugiewicz, a Director at Vistelar, often says, “The best way to avoid a fight is to never start the negative dance.” By training everyone according to the five approaches to showing respect, the Showtime Mindset, and the Universal Greeting (all discussed in later chapters), we can begin to establish an environment of care that is incompatible with anti-social behavior and violence.
Step #4: Train providers and staff to perform de- escalation skills.
Whether we like it or not just about everyone who walks into a hospital doesn’t want to be there. Most people walk in the front door with four or five problems. They are sick or someone they love is sick. They are missing time from work. They don’t have insurance or have high deductibles. Their spouse is unsupportive when they are sick or when one of the kids is sick. Some have other kids at home that need their attention. So many other possible stressors can pile on top of a hospitalization: pain, fear, health problems, financial problems, relationship problems and professional problems.
Little wonder there is a lot of violence in healthcare, but the potential for violence exists in many other professions as well, such as prison work and even banking. All these issues are just part of the picture, but they are a significant part. By training staff to recognize the signs of crisis, pre-attack postures, STAMP and gateway behaviors, we can arm them to make on the spot safety assessments and “change gears” in their approach.
For example, in Vistelar’s Point of Impact Crisis Intervention program students are taught to reduce stimulation, separate and support, adapt communication, and manage unmet needs—quickly and safely in order to de-escalate people in crisis. Untrained or insufficiently trained people tend to do what comes natural when they attempt to de-escalate people in crisis. And what they naturally do is get too close, talk too loud, and say too much.
Step #5: Adopt a zero-tolerance policy for violence and clearly define zero-tolerance.
Zero-tolerance does not mean that we throw everybody out who yells or curses in a hospital. It does require that we consistently address issues, like cursing and yelling, when they are first observed. If we can’t effectively and reasonably reign in uncooperative, anti- therapeutic, and anti-social behavior, then clear consequences have to be presented and enforced. When we are threatened or attacked, those consequences have to include loss of visitation rights and police involvement. In some cases it will even require refusal of service to patients. Healthcare is the only profession I know of where its customers can threaten or even assault workers with impunity. That has to change.
That said, people in crisis behave badly sometimes. First we must start by teaching staff to recognize crisis behaviors and distinguish them from anti-social behaviors. People in genuine crisis, who are yelling and otherwise acting-out may be reacting to medication, bad news, pain, and psychiatric conditions. These patients need privacy and support. Nonetheless, violent assaults generally should be reported to the police, even when they are the result of a crisis. The medical profession will become a lot safer when it more effectively partners with the law enforcement profession to determine criminality. The determination about whether criminal charges are appropriate are best determined after an investigation, not at the point of impact.
Injuries often occur when patients are in altered states of consciousness, such as when coming out of anesthesia. Many other patients suffer from brain injuries and brain-based disorders that can cause them to act-out. Healthcare workers must be trained to recognize, safely stabilize, and disengage from acting-out patients— and, if they are, fewer injuries will occur. In a recent Interventions for Patients with Challenging Behaviors course, a nursing supervisor said, “If I had known these skills last week, one of my nurses wouldn’t have been injured. I’m certain of it. I would have known what to do to keep us safe.” Just a couple of weeks after that, she was able to fulfill that prediction, as she reportedly led her team to safely stabilize a violent patient on her unit. Fortunately, this time no one was injured, including the patient.
Step #6: Train to persuade and educate patients in evidence-based practices.
Another one of the core skills discussed in this book is the Persuasion Sequence, which is founded on Vistelar’s five approaches to showing respect (covered in the next chapter). Just as with the angry biker, medical workers can use it to persuade patients to cooperate and even collaborate with proper medical care.
First, clinicians are trained to ask someone to cooperate, in a confident and professional tone of voice, while wearing the appropriate expression. Then they are trained how to set context, or explain why it’s in their interest to accept sound medical advice.
When done well, most patients will cooperate. If not, students of Vistelar’s conflict management methodologies are trained to offer choices or present options. When providers effectively help their patients to understand the benefits of recommended therapy versus the dangers of inaction, most patients will choose the right option.
It takes training and practice to lock-down context for uncooperative or fearful patients and loved ones, but it can be done reliably by trained communicators. For those patients who still refuse to cooperate, providers can confirm their intentions by offering them another chance to comply. When unsuccessful, providers have to be clear on their limits. No provider should ever prescribe a drug they know might be harmful to a patient. And when patients behave in a way that is detrimental to their health and the health of others, providers must be willing to Take Appropriate Action, up to and including discharging them from their practice.
Step #7: Make clear to everyone their right to protect themselves and their responsibility to protect patients in their care.
Many human service workers honestly believe they do not have the right to protect themselves or their clients, because they’ve been told throughout their career to never touch a client without permission— no matter what the circumstances! This belief is obvious nonsense to some healthcare professionals, but it’s an absolute truth to others.
The right to self-protection is an inalienable human right and no state can make a law taking away the right to self-protection. Although many institutions have flirted with the issue, no hospital, nursing facility, group home or other employer can enforce a policy that infringes on an individual’s right to self-defense, anymore than they can ask them not to breathe! Also, no one can avoid the responsibility to protect patients in their care. Sometimes that means going hands-on. What should medical workers do if their patient is about to swallow a bottle of pills, just watch? Ask some medical workers that question and you may get some surprising answers.
Many people, who work outside the healthcare field, would be shocked to learn how little training nurses receive in even the most basic stabilization skills, such as stabilizing a combative patient in the supine position. And that’s despite the fact that more injuries result from combative patients than from errant needle sticks! Therefore, due to the alarming rates of violence in hospitals and the responsibility for healthcare workers to care for people in distress, it is an absolute necessity to train medical workers in basic self- protection and stabilization skills.